 |
| It's not fun to acknowledge when you are having "urine problems". I find it to be one of the most silent and life inhibiting issues I face with FMS. |
There are many, many co-occurring issues that can come with Fibromyalgia (FMS). Interstitial Cystitis (IC) is one of them that isn't mentioned much in the FMS community. I was diagnosed with IC about 15 years ago, when I was 40. However, I believe I've had some level of IC for most of my life.
In the article Fibromyalgia and Related Conditions written by Dr. Daniel Clauw of UofM for the Symposium on Pain Medicine in 2015, he states, "Nearly all individuals eventually diagnosed with FM have several bouts of chronic pain in other regions of the body earlier in their life." Among the long list of comorbid issues interstitial cystitis/painful bladder syndrome. He explains, "This disorder often begins in childhood or adolescence, and individuals who eventually go on to develop FM..."
 |
| I don't have all of these symptoms and compared to some, my issues are moderate. However, its impact on my daily life and self-perception has been damaging. |
IC Progression
As a child, I hated taking time out from life to use the bathroom. I prided myself on how long I could go without peeing. To do that, I didn't drink much. Back then, there wasn't talk about drinking water and certainly wasn't a concern in my family. However, this penchant for not going to the bathroom, during my elementary years, combined with my people-pleasing ways would sometimes lead me to have accidents on my way home from school because I hadn't wanted to miss anything that was going on in class.
As a teen and a female, I was acutely aware of my weight and body image. I always felt overweight and was conscious of what I put in my mouth. Back then I remember thinking and even saying that, "I rather eat my calories than drink them." While this isn't all that bad in theory, it didn't mean I was drinking water. To me, water made me gag (I was that unused to drinking it). So, what it meant was that I didn't really drink much at all. What I did do, though, was to eat a lot of fruit, mostly canned back then.
Then, I began my teaching life. My doctor at the time said that it was very common that teachers had urinary tract infections and bladder infections because they were infamous for not drinking water and not being able to go to the restroom as needed. At this time in my life, I went from UTI to antibiotics, to yeast infection, to UTI sometimes leading into a bladder infection, to antibiotics, to yeast infection,...over and over and over. There was a time when I found myself going to the doctor every couple of months. One odd thing, though, was often, the "infections" were found out to be false when the urine test was finally completed a few days after I had already started the antibiotics. At that point, the doctor would always tell me to finish them "just in case" which I dutifully did.
It wasn't until I started having severe urgency and frequency (at this point I had finally learned that drinking water was important and had come to enjoy it) that led to a few embarrassing accidents at school that I went into an OBGYN doctor who also specialized in Interstitial Cystitis. At the age of 40, I was diagnosed with IC, after umpteen misdiagnosed infections.
As far back as I can remember, I had an aching in the area below my belly button. What made it feel better (and still does to a degree) is pressure and warmth. To my husband's chagrin, I was the clingiest spooner at night (when I most noticed the aching). His cute booty provided the exact pressure and warmth to calm the ache and let me sleep. I didn't know that ache was due to a problem with my bladder.
Been There. Done That
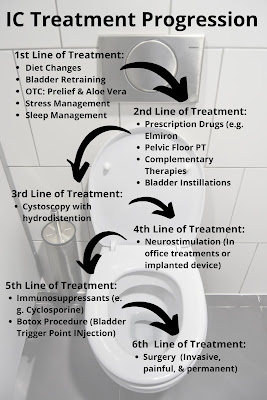 |
| I've done all (multiple times) but the last line of treatment, and I am determined NOT to go there! |
I have no affiliation or kickbacks for mentioning
any of the products in this post.
I am writing about my experiences only.
In addition to medication, I adjusted my diet as much as I could. I eliminated coffee (mostly due to the acid). There are some chicory and low acid coffees, but I have not found any locally. I have always been a semi bland eater due to acid reflux, so I have mostly stayed away from acidic fruits. However, with me being lactose intolerant (I could eat a piece of cheese and be cleared out for a colonoscopy), giving up all things tomatoes is nearly impossible. And I also refused to give up wine. These non-concessions are when I use Prelief.  |
| You'll note that most of the "good stuff" is on the avoid list😢 |
Besides, the pain, the frequency (especially in the morning) and urgency (which comes up strongly and seemingly out-of-the-blue) was the most embarrassing and difficult issue I had to contend with, especially at work. As a teacher, even when we are all having a break, students would invariably want to talk to me individually during this time. Some would even follow me to the bathroom, and I'd have to finally say, "Excuse me" and hedge my head towards the staff bathroom's door, for them to realize I had to use the loo.
I have used four types of prescription medication to alleviate frequency: Enablex, Tofranil, Myrbetriq, and Vesicare. These caused symptoms that were not fun: constipation, fatigue, dry mouth, dizziness, headaches, nausea just to name a few. And in the end, they didn't really seem to make a huge difference which I only found out after I got the courage to stop taking them.
For pain and the frequency/urgency issue, I have gone to four different pelvic-floor physical therapists. For someone who had planned what she would wear for her first delivery (for the 2nd, I knew better) and was too inhibited to get a massage from a stranger, this was really a step of desperation and a major lesson on not giving a damn. During my third stint of physical therapy, my urologist suggested botox injections at the trigger points in my bladder. This was an outpatient procedure that did involve me going under anesthesia. Sadly, I had no change in my symptoms.
My last PT suspected I had a labrum tear in my left hip; she said that she had been finding a connection between IC and hip-labrum tears. She, then, referred me to a specialist who after an MRI verified that this was the case, so I had the surgery.
 |
| Insterstim is a device that sends electrical stimulation to the sacral nerve, which is thought to normalize neural communication between the bladder and brain and between the bowel and brain. |
Being, in the end, these did not make much of a difference in my IC symptoms, I went to see another urologist who suggested it was time to implant an Interstim which a device the size of a quarter. This surgery was outpatient with local anesthesia only. I have a one-inch scar near the top of my left glute and a smaller incision at the sacrum. This healed up easily and being I did it during spring break, I didn't have to have any time off from work. There is a remote control that can change the level of stimulation delivered as well as change the program which determines the direction of the electrical pulse. I tell people, "It's like a pacemaker for my bladder."
This implant seemed to really help for a bit over a year (I had it two years ago). However, I began to have site pain in my left glute and was having ongoing sharp pain in my left psoas which became convinced was coming from the electrical stimulation and my crazy Fibro-amplified nervous system. I chose to turn it to zero for about three months. During those months, with chiropractor adjustments, medical massage, and yoga, the sharp pain went away. I was set on getting it removed.
However, after seeing my urologist, and hearing what the removal would be like (not as easy as the implant surgery), we came up with a retry. She reprogrammed the device and set me up with new physical therapy which I have just started.
 |
| Getting tired of having to know the whereabouts of every bathroom wherever I am. |
And so, I am working on retraining my bladder which in the end is just like retraining my brain with an addition of a few exercises. My goal is to be able to comfortably go on upcoming hiking trips (in which restrooms are not readily available and dropping into a squat in the woods isn't fun to do every hour.)
Helpful IC Resources:
Thank you for visiting my blog today.
I am committing to posting once a week on Fridays.
However, as you know, my new normal means that sometimes I have
to listen to my body and am not able to follow through as planned.
Thank you for your understanding.
Click link Subscribe to Pain FULLY Living Weekly Posts by Email





This was very interesting. I am sorry you are suffering so. I have always got frequency of urination but put it down to diabetes and fibro. Maybe it's IC. I will look into it. Thanks for sharing.
ReplyDeleteI was surprised to find the connection between IC and FMS. Not sure why because it seems like much of my other issues is connected.
DeleteI was misdiagnosed with IC because of my fibromyalgia diagnosis. My UITs were caused by my pain medication and frequent urination was the result of having my bladder pulled and attached to my sidewall by endometriosis adhesions. Thankfully, I fought my diagnosis and the real culprits were finally found. I always suggest getting a second opinion to be safe.
ReplyDeleteYes, for sure. Glad you pushed to find the correct diagnosis. For me,the IC came 15 years before my FMS diagnosis. Wasn't until I began to research IC and FMS, that I found that they are often connected.
DeleteVery interesting! I only recently learned about this condition, and this is a very informational post.
ReplyDeleteI'm glad you found it informative. This is a condition that doesn't seem to be talked about a lot.
DeleteI swear, IC is the absolute worst. It took me years to find out that's what I had. Mine flares up when I'm under a lot of stress (aka a pandemic) and there's nothing I can do except try to be less stressed.
ReplyDeleteYes, stress is a huge contributor to all my IC symptoms. Breathing, yoga, meditation helps. But as a young mom and full time teacher, when first diagnosed, this wasn't something i knew about and I doubt i would have taken the tome for myself if i had. So many demands. I've done all these changes after being forced to go on long-term leave and retire. I sure hope that you can somehow incorporate self care. I feel for you.
DeleteI started writing a blog post on this yesterday. My painful bladder syndrome diagnosis is very new so I learnt so much from this post of yours. Thank you for sharing this.
ReplyDeleteI'm so glad this has veen helped you, Shruti. If you have any questions, just contact me. However, all you are doing with meditation and breathing will help.
DeleteWhilst I don't have these conditions, I do get bladder and vulva irritations from the dryness of Sjögren's syndrome, and sometimes I do think they're worse than pain itself. I spend all night pacing up and down just hoping for some relief, but nothing helps. Thanks for sharing your knowledge and experience so it helps others out there.
ReplyDelete